
Osteochondroma
What is osteochondroma? -Osteochondroma Surgery
Osteochondroma is a benign, non-cancerous bone tumor that develops in childhood and adolescence. It is an abnormal development that occurs on the bone surface next to the growth plate in the bone. Growth plates are areas that allow cartilage to develop at the ends of long bones. Bone growth occurs through the growth plate, and when the child is fully developed, the growth plates harden and turn into normal bone. Osteochondroma is a tissue made of bone and cartilage formed by the excessive development of the growth plate. It is normal for osteochondroma to grow during the child's skeletal development, but after the skeletal development is completed, osteochondroma growth stops.
Osteochondroma Treatment
In many cases of osteochondroma, no treatment is required other than regular check-ups. However, if changes in the character of the mass are observed or complications occur due to vascular nerve compression, surgery may be required. Osteochondromas can develop as a single tumor (osteocartilaginous exostosis) or multiple (multiple osteochondromatosis).
Osteochondroma Surgical Treatment
Your doctor will consider surgery if you have the following symptoms:
- Pain
- Nerve or vascular compression
- Presence of a wide cartilaginous cap
During surgery, the mass is removed down to the normal bone level.
Osteochondroma Surgery Recovery Time:Return to daily activities usually takes 3-6 weeks, although it varies depending on the size and location of the mass.
Single-Solitary Osteochondroma: It is the most common bone tumor, accounting for 40% of all bone tumors. It is not cancer and does not spread far.

The cause is unknown, it is not related to injury, but it is thought to be related to the gene called EXT 1. Since the cause is unknown, it is not possible to prevent it. Osteochondromas are often diagnosed between the ages of 10-30.
Multiple Osteochondromatosis: Other names are multiple exostosis, multiple hereditary exostosis, familial osteochondromatosis, multiple hereditary osteochondromatosis and diaphyseal achalasia. In advanced cases, bone developmental abnormalities, short stature and forearm deformities may be observed.

In this syndrome, the change of benign mass to worsening is more common than single osteochondromas. While the cause is familial-genetic in 70% of the cases, it develops spontaneously in 30%.
Orthopedic Oncology Evaluation:If you or your child shows signs of developing into cancer, you should see an orthopedic doctor who specializes in bone tumors.
Symptoms of Cancer:
- Growth of osteochondroma after puberty
- Pain around the mass
- A cartilage cap wider than 2 cm
In this case, MRI and CT should be performed. If necessary, a lung CT is performed for suspicion of metastasis. If your doctor deems it necessary, a biopsy taken from the mass will support the diagnosis of cancer. When it turns into cancer, it often turns into the type called chondrosarcoma.
Aneurysmal Bone Cyst-Simple Bone Cyst
What is a Bone Cyst? Bone Cyst Treatment: Simple Bone Cyst:It is a common benign bone lesion. It is often seen in children and is usually asymptomatic. They are usually first seen within the age of 20. 65% of the cases are under the age of 18, the average age of diagnosis is 9 years. They are 2-3 times more common in boys than in girls. Active cysts are often seen between the ages of 1 and 10. These cysts often do not cause symptoms and are detected incidentally, but in some cases, pain, swelling and limitation of movement in the nearby joint may occur. The most common referral to the doctor is due to an unexpected fracture. The cause and mechanism of the disease are unknown. In the active phase of the disease, the cyst becomes adjacent to the growth plate, and as it becomes inactive, it moves away from the growth plate, that is, normal bone forms between the growth plate and the cyst, and the cyst usually disappears with age. While the diagnosis of simple bone cyst is usually made by direct radiography, tomography and MRI may be required for differential diagnosis. Simple bone cysts are typically located intramedullary. Active cysts are located in the long bone metaphyseal region and rest on the growth plate.
- Proximal humerus is the most common 50-60%
- Proximal femur 30%
- Other long bones
Locations other than this are rare and usually occur in adults
- The spine is usually the posterior elements
- The pelvis is only 2% in size
- Calcaneus heel bone
On plain radiography, they are lucent lesions with well-circumscribed geographical character. A narrow transition zone is seen. It is usually seen in patients with incomplete skeletal development. It is located in the center of the bone. There is a thin sclerotic rim. No periosteal reaction or soft tissue component is observed. They generally expand the bone and thin the bone membrane, but if there is no pathological fracture, they do not perforate the cortex. Simple bone cysts are often unilocular, although pseudotrabeculation may occur. True trabeculations are only seen if recurrent fractures have occurred. If there is a fracture within the lesion, a loose bone fragment can be seen and this image is called the falling leaf sign.
CT: It is useful in detecting fractures that are not visible directly in graphite and can also be used to evaluate the content of the cyst.
Emar: Fluid-liquid levels can be seen. If there is a fracture, signal heterogeneity, periosteal reaction and soft tissue edema may occur.
Simple Bone Cyst Treatment: Treatment is usually not required for asymptomatic lesions. If the lesion is very large and poses a risk of fracture or causes deformity, intracystic steroid injection can be applied to the arms. If the cyst is in the hip bone, curettage and bone grafting may be required. It differs from NOF and aneurysmal bone cysts in that it is centrally located, and it differs from giant cell tumors in that the cyst does not reach the joint surface and is seen at young ages. Additionally, it may be necessary to make a differential diagnosis with fibrous dysplasia cysts, intrabony lipoma and ganglion.




Aneurysmal Bone Cyst: Bone cyst surgery:
They are benign, expansive, lytic, cystic masses rich in osteoclastic giant cells. They are frequently seen in children and adolescents. 80% of the cases are under the age of 20, but it can occur at any age. There is no gender difference. Diagnosis is made by radiology and biopsy.
- Multicystic mass accompanied by fluid levels
- Pathology in which cyst walls contain findings such as fibroblasts, osteoclastic giant cells and hemosiderin pigment, new bone formation
- USP6 gene is present in 60% of cases
Aneurysmal Bone Cyst Symptoms: Pain and swelling. Rarely, pathological fracture may occur. If it settles in the spine, it can cause nerve compression. The location is usually in the bone metaphysis and eccentric, adjacent to the growth plate.
- Most common in long bones (65%), especially femur, proximal tibia and fibula and humerus
- In the spine and pelvis (20-30%). In 40% of the cases, the posterior elements protruding into the vertebral body and the obturator region of the pelvis
It becomes central when located in short bones.
Although fluid levels on MRI are characteristic of aneurysmal bone cysts, they are never pathognomonic. It should be noted that fluid fluid levels can be seen in both benign (giant cell tumor, chondroblastoma, simple bone cyst) and malignant (telangiectatic osteosarcoma) tumors.
Aneurysmal Bone Cyst Treatment: Benign Bone Tumor Treatment:
Although they are benign, they can show various clinical presentations: they can be silent, active or aggressive. In the treatment, curettage (scraping) or excision (complete removal) and grafting (bone powder) are performed. If the bone is weakened, it is supported with metal plates, nails and screws.

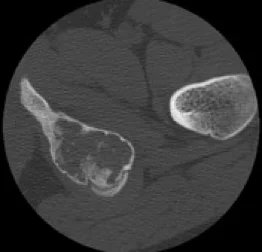
Picture 7: Aneurysmal bone cyst at the upper end of the tibia.
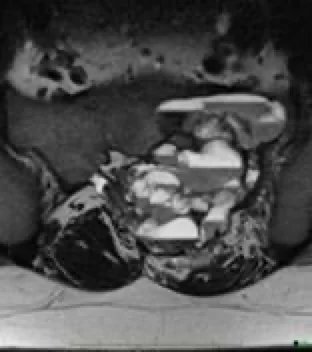
Picture 9: Pelvis Aneurysmal bone cyst.
The risk of recurrence may increase to 30% depending on the treatment method.
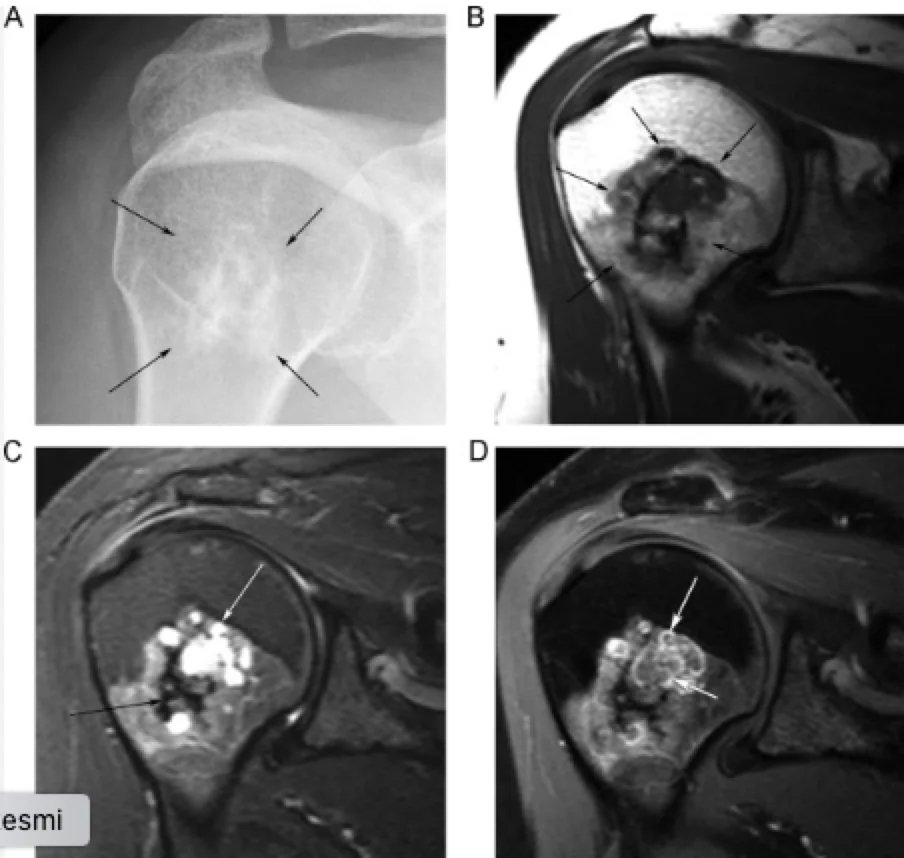
Osteoid Osteoma
Leg Tumor Symptoms: Osteoid Osteoma Treatment: Osteoid osteomas are benign bone-forming tumors that usually occur in children (especially adolescents). They have a characteristic nidus (1.5 or 2 cm) and surrounding osteosclerotic reaction, typically causing night pain and relieved by the use of NSAIDs (painkillers). Osteoid osteoma is usually found in children, adolescents, and young adults between the ages of 10 and 35. They constitute ~10% of all benign bone lesions and are 2-4 times more common in men than in women. They are the classic cause of painful scoliosis of the spine, where the curvature is concave on the side of the lesion. This typical appearance is seen in more than 75% of spine cases. Soft tissue swelling due to the tumor may occur, and if the tumor is close to the growth plate, faster growth may occur on that side, possibly associated with hyperemia. It is more likely to mimic joint inflammation (inflammatory arthropathy or synovitis) when the lesion remains within the joint capsule. Joint effusion is often present in these cases.
In Which Bone Does Osteoid Osteoma Occur? Most osteoid osteomas occur in the long tubular bones of the extremities (especially the proximal femur), but any bone can be involved.
- Long bones of the limbs: ~65-80%
- Most commonly femur (especially femoral neck)
- Mid-tibial diaphysis
- Phalanges: ~20%
- Vertebrae: ~10%, predominantly posterior elements

Also, osteoid osteomas are usually cortical lesions but can occur anywhere in the bone, including medullary, subperiosteal (most commonly in the talus), and intracapsular. In intracapsular osteoid osteomas, the periosteal reaction may occur away from the lesion itself.
Osteoid Osteoma Diagnosis: Plain radiography:
The radiograph may be normal or may show a solid periosteal reaction with cortical thickening. The nidus can sometimes be seen as a well-circumscribed lucent zone, sometimes with a central sclerotic spot. However, extensive sclerosis can sometimes obscure this focus.
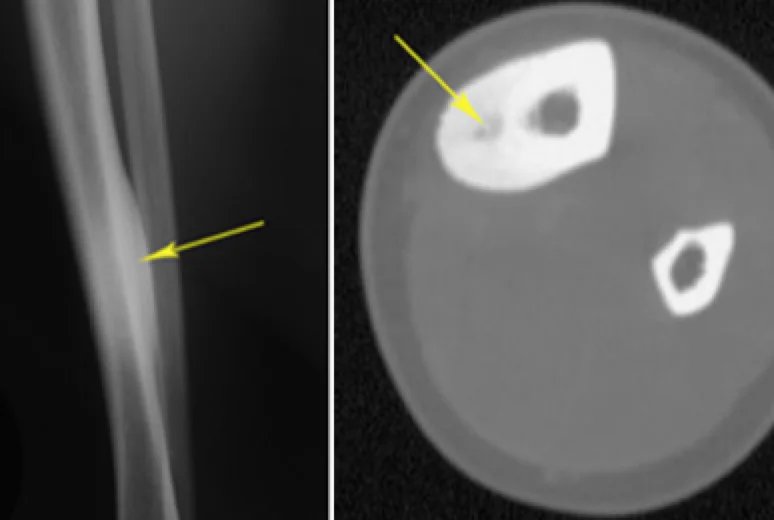
BT:
CT is excellent at characterizing the lesion and is the method of choice. It typically shows a focally lucent spot within surrounding sclerotic reactive bone. A central sclerotic spot may also be seen.
MRI:
Although MRI is sensitive, it is nonspecific and often cannot identify the focal point. The pattern of hyperemia and resulting bone marrow edema may lead to scans being misinterpreted as representing aggressive pathology. The signal intensity of the nidus and the degree of contrast enhancement are variable in all sequences. In patients without a history of lower extremity overuse, determination of the half-moon sign is highly specific and sensitive for detecting osteoid osteoma of the femoral neck. In these cases, the half-moon sign must be detected on fluid-sensitive MRI sequences. In cases of excessive use (e.g. marathon runners, members of the armed forces), the half-moon sign may indicate a stress reaction/fracture.
Nuclear Medicine:
Bone scintigraphy will show typical focal enhancement and occasionally a double density sign (also known as a less hot spot within a hot area); this is highly specific if present and is helpful in differentiating osteoid osteoma from osteomyelitis.
Osteoid Osteoma Treatment:
The lesion is benign and its treatment is traditionally surgical resection. Historically, this has sometimes been difficult due to the inability to locate the nidus at the time of surgery. Percutaneous methods are also used in selected cases instead of surgery.
Lesions Confused with Osteoid Osteoma: Differential Diagnosis
- Osteomyelitis (e.g. Brodie's abscess): A bone scan shows a central area of decreased uptake, representing an avascular area of purulent material.
- Osteoblastoma: >1.5-2 cm in size
- Stress fracture
- Cortical desmoid
- Osteochondroma
- Osteosarcoma
- Bone island
- Localized cortical thickening
- Intracortical hemangioma
- Reactive sclerosis around the osteolytic lesion
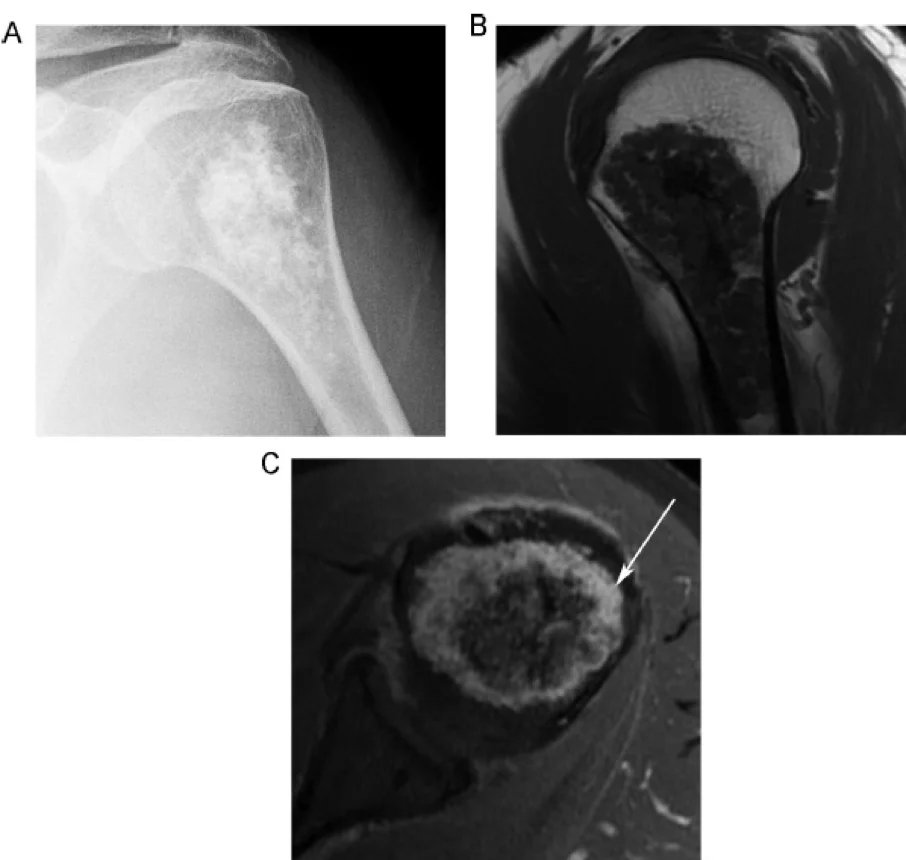
Enchondroma
Enchondromas, also known as chondromas, are common intramedullary hyaline cartilage neoplasms that have benign tumor characteristics on imaging. They share histological features with low-grade chondrosarcoma and are sometimes classified under the umbrella of low-grade chondral tumors. It is most commonly diagnosed in childhood-early adulthood, with the highest incidence occurring between the ages of 10-30. It is the most common primary benign bone tumor of the hand and wrist. It constitutes ~5% of all bone tumors and ~20% of benign bone tumors.

Enchondroma Diagnosis:
The presence of abundant cartilage matrix and the absence of cellular atypia/mitosis, soft tissue extension and cortical invasion are diagnostic criteria.
Enchondroma Symptoms:
Enchondromas are often detected incidentally, and this is most important in order not to confuse the tumor with more aggressive lesions. As a rule, enchondromas should be asymptomatic; however, hand/foot lesions may present with pathological fracture or pain from impending fracture. Malignant transformation to low-grade chondrosarcoma is rare, and when it occurs it may present with pain.
Enchondroma Pathology:
Enchondromas consist of lobules of mature hyaline cartilage surrounded partially or completely by normal bone. Cartilage lobules may undergo endochondral ossification, often resulting in the characteristic 'rings and arcs' mineralization pattern. They arise from growth plate cartilages/chondrocytes that have become isolated within mature bone. Therefore, they can be seen in any bone composed of cartilage. By definition, they do not show any histological evidence of local invasion (differentiation from low-grade chondrosarcoma). However, it is important to be aware that enchondroma cannot be reliably distinguished from chondrosarcoma by histology and that diagnosis depends on the correlation of clinical, imaging, and pathology findings. Grossly, lesions are usually 3 cm, translucent, nodular, and largely greyish blue. Enchondromas are typically found in a central or eccentric location within the medullary cavity of tubular bones:
- Small tubular bones of hands and feet (~50%)
- Proximal phalanx is the most common
- Large tubular bones
For example. femur, tibia, humerus
Rarely, an enchondroma may extend throughout the cortex and exhibit an exophytic growth pattern. This is known as enchondroma protuberans and may occur sporadically or as part of Ollier disease.

Plain X-Ray And CT:
Enchondromas have a variable appearance but are typically small 5 cm intramedullary lytic lesions with non-aggressive features:
- A narrow transition zone
- Sharply defined margins
- +/- chondroid calcification (ring and arch calcification)
Hands/feet often have no matrix mineralization (purely lytic)
- +/- expansion
- More commonly in hands/feet, less commonly in long bones (tibia, femur)
- There may be mild endosteal scalding
- It should not “grow” through the cortex (unless there is a pathological fracture)
- No serious bone destruction
- No periosteal reaction
- No soft tissue mass
Most enchondromas occur more frequently in the metaphyseal region, probably because they originate from the growth plate. They are rarely seen in the epiphysis, and a cartilage lesion in the epiphysis is more likely to be chondrosarcoma. MRI is useful in evaluating soft tissue invasion and confirming the diagnosis. Enchondromas appear as well-circumscribed, somewhat lobulated masses that replace the bone marrow. Differentiating enchondroma from low-grade chondrosarcoma is problematic because they can have similar appearances.
Distinction from Enchondroma to Low Grade Chondrosarcoma:
Distinguishing between enchondromas and low-grade conventional chondrosarcomas is a frequent challenge because the lesions are so similar both histologically and radiographically. However, it should be noted that distinguishing between them can be a controversial issue, as both can be closely monitored clinically and radiologically or treated if symptomatic.
Radiographic Features:
- Size
Lesion size over 5-6 cm suggests chondrosarcoma.
- Cortical violation
Seen in 88% of long bone chondrosarcomas
It is seen in only 8% of enchondromas
- Deep endosteal fistula covering > 2/3 of the cortical thickness
Seen in 90% of chondrosarcomas
It is seen in only 10% of enchondromas
- Permeative or moth-eaten bone appearance
It is seen in high-grade chondrosarcomas.
- Soft tissue mass
It is not seen in enchondroma.
- Increased uptake on bone scan
It is seen in 82% of chondrosarcomas.
It is seen in only 21% of enchondromas.
- Location
Hands and feet are rare sites of chondrosarcoma. Outside of the hands and feet, chondrosarcomas outnumber enchondromas. The spine, pelvis, sacrum and ribs are places where enchondromas are rarely seen.
- Patient age
Enchondromas usually occur in young adults.
Chondrosarcomas tend to occur in middle-aged patients.
- Pain
Chondrosarcomas almost always present with pain.
Enchondromas are painless unless they cause a pathological fracture.
Enchondroma Treatment:
Since enchondromas are classified as Bone-RADS 1 lesions, they are typically considered benign and should be left alone if asymptomatic. The majority of enchondromas remain asymptomatic and do not require treatment. Pathological fractures are usually treated with curettage and bone grafting, and follow-up x-rays are taken to monitor healing and recurrence. A biopsy is taken before surgery. Recurrence is reported at a rate of 2-15% and is suggestive of malignancy.
Treatment is more aggressive if malignant transformation is suspected, which occurs in less than 5% of cases.






