Bone Tumors
An appropriate and effective study for bone tumors by the orthopedic tumor surgeon with his team (orthopedic tumor radiologist, orthopedic tumor pathologist, vascular surgeon, microsurgeon with sufficient reconstruction experience, radiation oncologist and medical oncologist) is essential for the patient's treatment to be adequate, otherwise the patient will be treated incorrectly. Diagnosis or delayed diagnosis will result in serious disabilities and death.
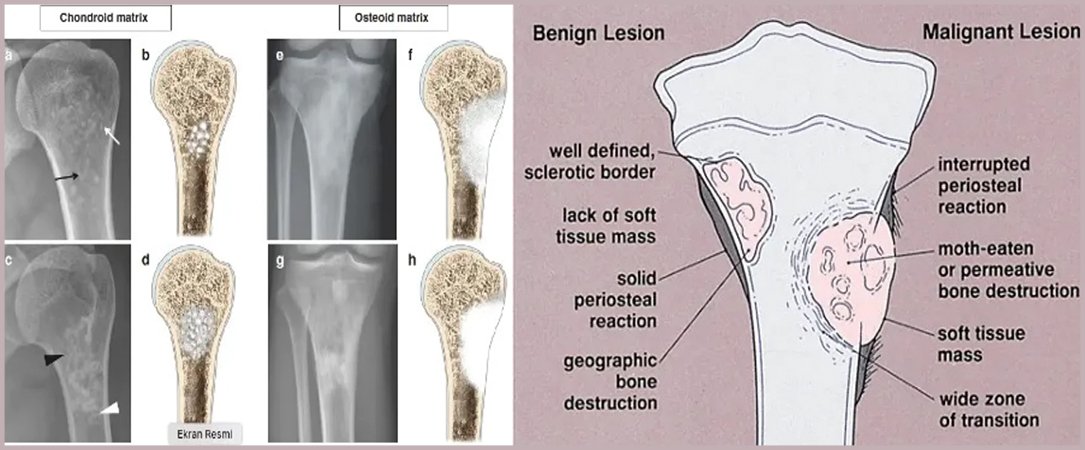
Diagnosis begins with taking a detailed history of the patient's complaint, a detailed examination and a classic x-ray. Benign tumors are generally seen as lesions that do not cause any complaints, have geographical features, sclerotic edges, and do not cause bone destruction or periosteal reaction.
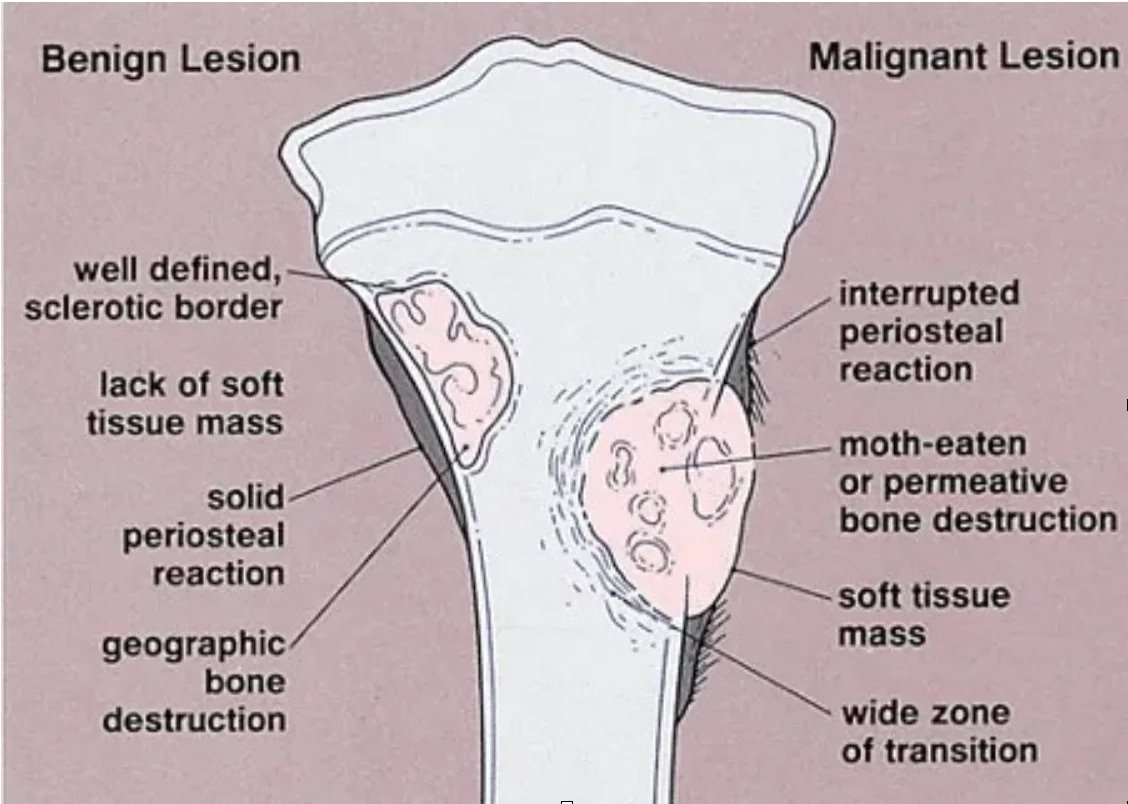
Malignant tumors, on the other hand, cause regional pain and show lytic, permeative growth and poor-vague borders with intact bone on radiographs. Bone membrane destruction and/or periosteal reaction (Picture 2) may be observed.
At this stage, a classical orthopedic doctor should refer his patient to a tumor orthopedic specialist. Advanced imaging and biopsy are methods to be decided by your tumor doctor.
Clinic of Bone Tumors
The clinic is very variable. Lesions in patients may occur accidentally or with symptoms such as pain and swelling. For example, fibrous dysplasia or osteochondromatosis may occur with bone curvature in patients. Fractures, soft tissue masses and swelling may occur along with the tumor in the bone. Painful lesions are generally seen in aggressive (benign but aggressive) and potentially malignant tumors. Since the clinical spectrum of benign and malignant tumors is very wide, diagnosis should be made by a physician experienced in tumor surgery. Incorrect and inadequate diagnoses and treatments will expose a patient who could be managed with simple follow-up or treatment to unnecessary, expensive and damaging tests and treatments. Likewise, inadequate diagnosis and treatment of aggressive and malignant tumors may result in loss of limbs or loss of life.
Clinic in Benign Tumors
There may be moderate pain that is relieved with painkillers. Pain occurs slowly and may be associated with activity or trauma. For example, night pain that responds to painkillers is typical in osteoid osteoma. Fractures that occur with a movement that would not normally break the bone are called pathological fractures. In some benign lesions, pathological fractures may develop with single or repeated traumas. IF THE LESION IS DETECTED ACCIDENTALLY WHILE THE PATIENT HAS NO PAIN OR SYMPTOMS, THEN THEY ARE MOST LIKELY BENEFICIAL.
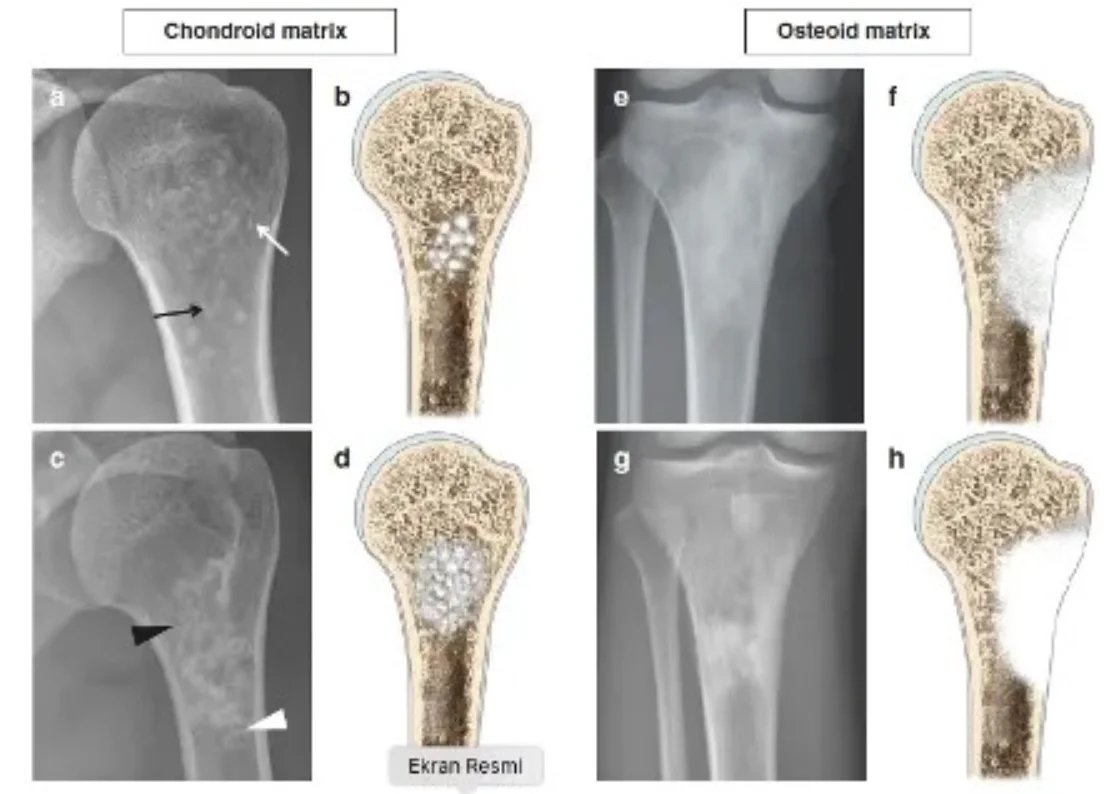
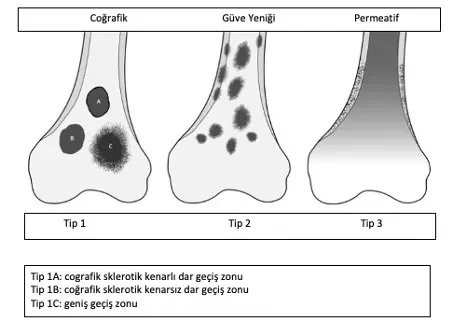
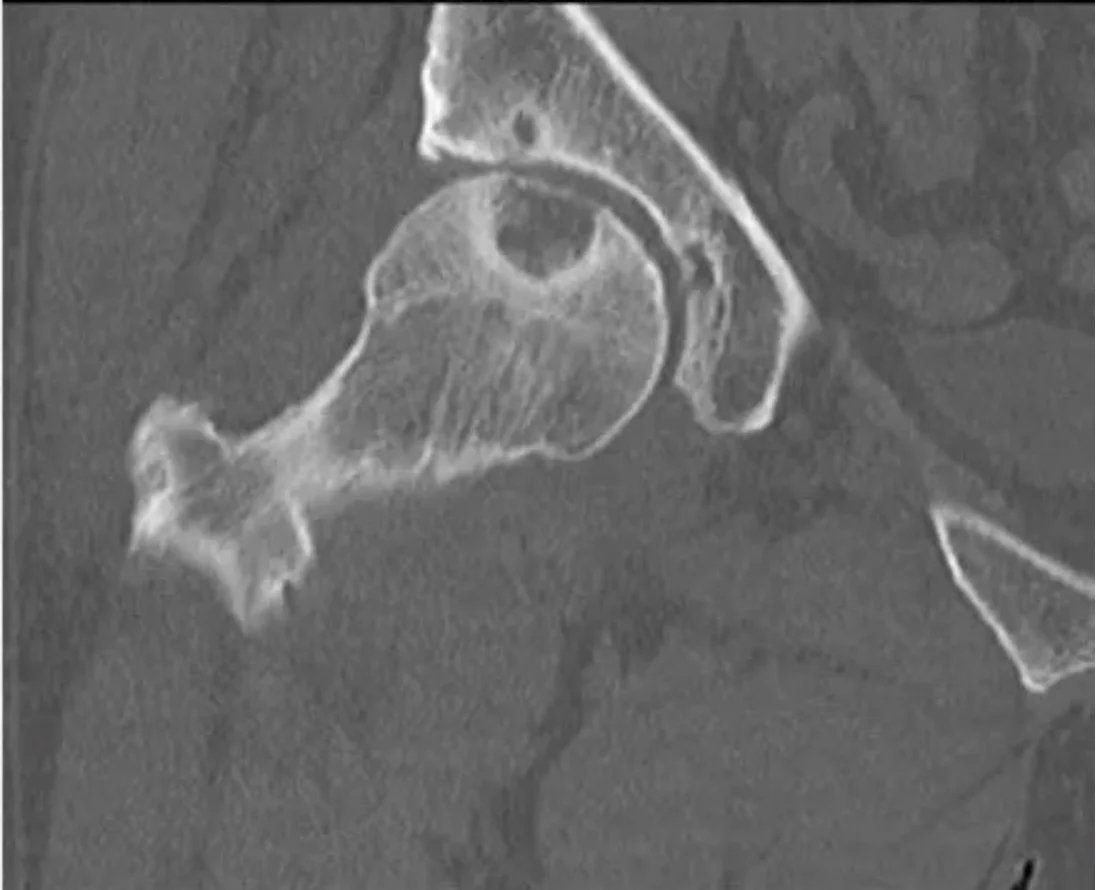
An experienced tumor surgeon will understand whether the lesion is good or requires a biopsy based on the patient's age, location of the lesion, and x-ray. Radiological examination should include the entire bone. Benign tumors are typically geographical, have narrow transition zones and sclerotic edges (Figure 1). Endosteal thinning may occur, but cortex destruction is rare. Another helpful criterion in diagnosis is the matrix of the lesion
Emar reveals the soft tissue component, contrast material retention, bone marrow edema and signal characteristics of the lesion. Scintigraphy is effective in poliostatic fibrous dysplasia, multiple enchondromatosis and histiocytosis to see multiple bone involvements. A cold scintigraphy does not indicate that the lesion is aggressive or non-malignant (e.g. multiple myeloma, renal cell carcinoma metastasis). Degenerative and overuse lesions in lesions adjacent to the joint are also included in the differential diagnosis.
If there is cortex destruction, permeative growth and periosteal reaction, further examination is essential. If the diagnosis is not clear despite CT and MRI, a biopsy is required. After the diagnosis of benign bone tumor is made, observation and follow-up can be done at 3-6 month intervals to ensure radiological stability. Surgical intervention will be required to stop bone destruction, detect pathological fractures or strengthen lesions that are about to break, and prevent deformities.
Clinic in Malignant Tumors
The clinic is very variable. Lesions in patients may occur accidentally or with symptoms such as pain and swelling. For example, patients with fibrous dysplasia or osteochondromatosis usually show signs of bone curvature. The pain is often severe and painkillers are not enough. There is a dull and deep pain unrelated to activity or rest. If a pathological fracture occurs, pain occurs suddenly. Numbness in the feet and legs, weakness, bowel and bladder dysfunction are seen in spine and sacrum tumors. There may be an accompanying swelling. Fatigue, weakness and fever may occur. Increased alkaline phosphatase, elevated calcium and anemia may be seen in the laboratory. Family history of cancer and sarcoma is important in the history. For example, retinablastoma, Li Fraumeni syndrome and Rothmund-Thompson syndromes have a predisposing effect on bone tumors such as osteosarcoma. It has been reported that multiple enchondromatosis lesions may worsen. In addition, sarcoma may develop in Paget patients, history of radiotherapy, chronic osteomyelitis and bone infarction. The biopsy should be performed by an orthopedic tumor surgeon because the biopsy should be done as closed as possible and this requires experience. In addition, the biopsy site should be chosen so as not to contaminate important vessels and nerves. The biopsy site must be on the line preferred by the tumor surgeon in the actual tumor surgery. Otherwise, long and heavy surgeries such as serious muscle and tissue losses, dangerous vascular transplants, nerve losses and skin transplants will be required. This may increase limb loss and shorten life expectancy. If a malignant bone tumor is diagnosed, staging should be done. For this, PET imaging must be performed quickly. In patients over 40 years of age, the lesion is usually metastatic carcinoma, multiple myeloma or lymphoma. In addition, the breast in women and the prostate in men should be evaluated and protein electrophoresis should be performed in serum and urine. Treatment may require a multidisciplinary approach, including radiation and medical oncologists, under the leadership of an orthopedic tumor surgeon. Fractures, soft tissue masses and swelling may occur along with the tumor in the bone. Painful lesions are generally seen in aggressive (benign but aggressive) and potentially malignant tumors. Since the clinical spectrum of benign and malignant tumors is very wide, diagnosis should be made by a physician experienced in tumor surgery. Incorrect and inadequate diagnoses and treatments will expose a patient who could be managed with simple follow-up or treatment to unnecessary, expensive and damaging tests and treatments. Likewise, inadequate diagnosis and treatment of aggressive and malignant tumors may result in loss of limbs or loss of life.






